MND is a rare neurological condition that affects that motor system, resulting in weakness and wasting of the muscles. It is degenerative and progressive and life shortening. The MND Association estimates that there is a 1 in 300 risk of getting MND across a lifetime and it usually occurs between 50-70 years of age. (MND Association, 2018).
the muscles. It is degenerative and progressive and life shortening. The MND Association estimates that there is a 1 in 300 risk of getting MND across a lifetime and it usually occurs between 50-70 years of age. (MND Association, 2018).
The condition affects that nerves and cells of the brain, spinal cord and peripheral nerves that control the muscles in the body. It affects every movement we perform including to communicate, eat and drink, move and walk, manipulating objects and breathing. Some also experience difficulties with cognition (thinking) and behaviour. It affects everyone differently and can be difficult to predict due the variability of speed of progression. Because it is not that common, it is important that individuals seek out and can access specialists who can best support them in the management of their condition, maintenance of quality of life and optimisation of function. The multidisciplinary team approach can improve survival with effective and timely interventions and communication between teams.
There are different types of MND and the progression of the condition varies on the type. Examples of these include:
- Progressive muscular atrophy (PMA)
- Progressive bulbar palsy (PBP)
- Primary lateral sclerosis (PLS)
- Amyotrophic lateral sclerosis (ALS) – this is the most common and affects approximately 85% of those diagnosed (Kent, 2012)
The initial symptoms of Motor Neurone Disease include:
- Spasticity of the muscles (cramps and spasms)
- Muscle twitching
- Difficulties with speech, swallowing and saliva management, observed by possible drooling
- Muscle weakness that may affect initially effortful tasks (climbing stairs, lifting something heavy)
- Muscle wasting (often first noticed in muscles in one hand, arm or leg)
- Falls or clumsiness
Extreme fatigue, pain and breathing difficulties can occur as the condition progresses.
Due to the life-shortening and progressive nature of the condition it can be challenging to continuously adjust to the changes to independence and the ability to carry out every day activities. Engagement in rehabilitation services requires individuals to have autonomy in choice and trust in healthcare professionals who are knowledgeable about the condition, can offer reassurance and can appreciate their experienced loss (Foley, Timonen, & Hardiman, 2014) and the future experiences of their significant others and carers (Harris, 2017) . The importance of emotional support should be inherent in therapeutic approaches to support individuals with MND to ensure that care and support suggested and offered is right for the individual (Harris, 2015). Quality of life affects decisions made relating to clinical and therapeutic interventions that may be required (Lemoignan & Ells, 2010) and this quality of life includes relationships, environment, personal well-being, engagement and coping.
When considering the clinical and functional management of MND, therapists need to be mindful of 24-hour positioning. Tone management requires optimal positioning, and individuals may require orthotics for upper and lower limbs. Nociceptive pain reported by MND clients (Lau, Brennan, & Gardiner, 2018) may need body parts to be well supported and protected. Mobility aids may need a gradual introduction to promote acceptance and familiarity, however these may also be required within a short period and it is vital that these allow for self-expression and that mobility aids can respond to changing level of acceptance and need.
A wheelchair will be required for mobility and will need to adjust to the individuals function and physical changes during the course of this condition. Powered wheelchairs may allow for increased engagement in community activities and greater satisfaction of users, however may be less portable – wheelchair solutions should be as comfortable and easy to use as possible, whilst remaining easily adaptable (Arbesman & Sheard, 2014).
When considering seating provision for individuals, the key elements need to include:
- Optimise autonomy and independence in engagement within chosen activities.
- Adaptability and ease of adjustment.
- Be easy to use by client and family/carers.
- Providing support and positioning to minimise fatigue and pain.
- Be aesthetically pleasing and allow for self-expression.
- Supporting the body to maintain a healthy alignment against gravity at the hips, trunk, and head.
- Allow for independent and assisted transfers, as appropriate.
- Optimise positioning for vital functions (e.g. breathing) and accommodate medical devices.
- Providing appropriate pressure relief and comfort.
- Adequate support to the pelvis and trunk to provide stability.
- Adequate support to the arms to reduce pain in the shoulders (Lau et al., 2018).
- Protection of body parts to minimise pain.
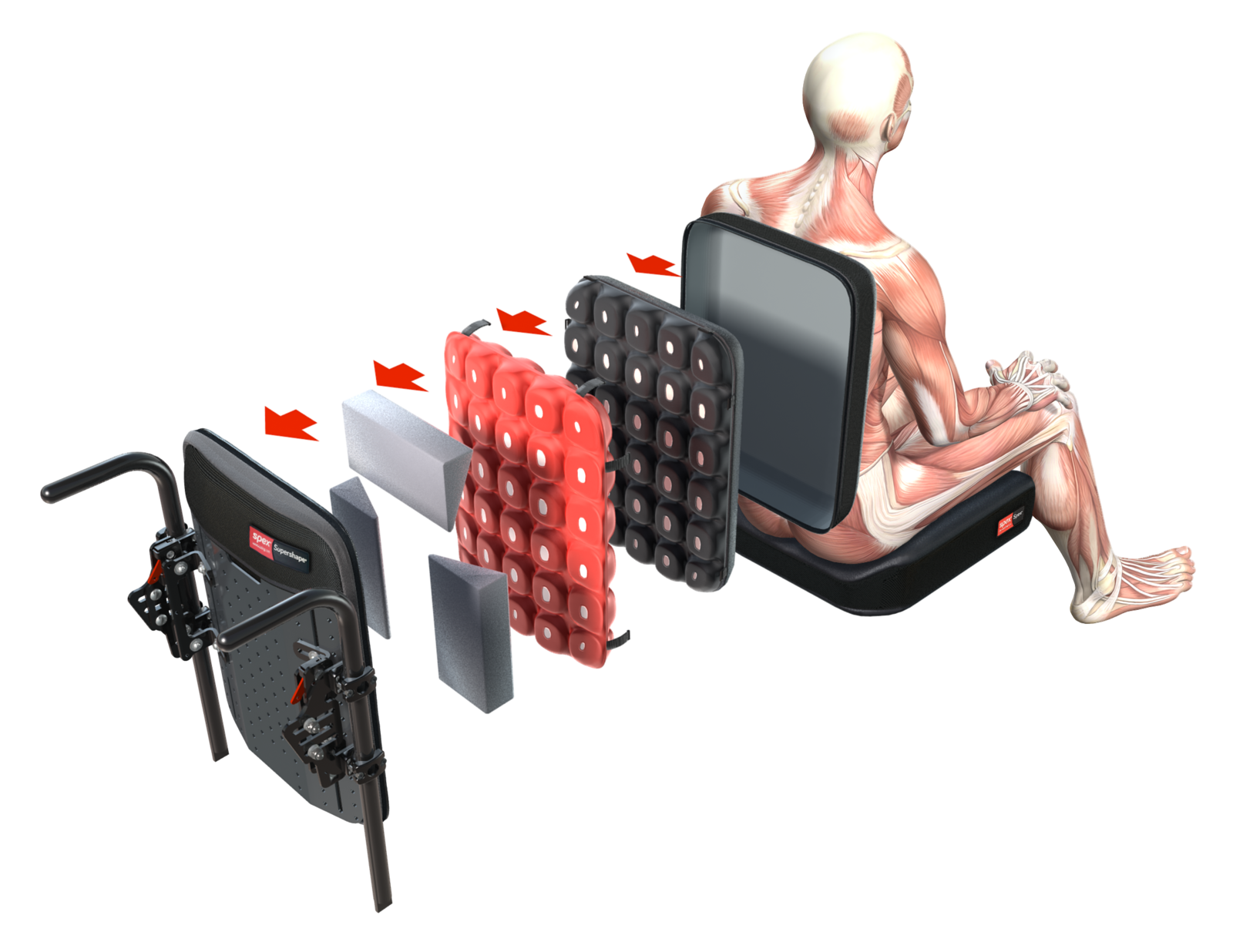
Spex seating is a versatile, adjustable modular seating system that can be fixed onto almost any wheelchair chassis and can adjust to the person’s changing needs.
chassis and can adjust to the person’s changing needs.
It is a modular seating technology system that includes cushions, hip supports, trunk supports, knee/thigh supports, head and arm supports, a variety of accessories, and back supports that can allow for easy adjustment and contouring and shaping within the components.
It can provide simple to complex postural support, whilst still allowing for easy transportation, as appropriate. The same seating system can be transferred between manual and powered wheelchair bases.
The seating options include simple options to optimise comfort, as well as more immersive and shaped options to accommodate the need for additional stability and postural support.
Users only need order what they need and can add/remove components or contouring (within seat and back cushions) as their condition changes. The accessories can be configured to optimise ease of use for both the person and carers.
Spex is customisable to reflect personal colour choice, quick to adjust and modular to provide the right support when needed.
Adjustments do not require specialist wheelchair clinics but can be done by locally trained therapists to optimise postural responsiveness to the users’ needs.
Spex shapes better lives and is highly customisable to meet individual need!
Spex accessories, cushions and back supports can be used in isolation or as a full seating system on their chosen wheelchair chassis. The Spex seat pan and backrest shell can be removed if the wheelchair and seating system needs to be transported in a vehicle (e.g. if fitted to a folding manual wheelchair).
The mix-and-match componentry allows for products to work together based on need, level and direction of support required and the user’s functional requirements. The seating options allow for active wheelchair use and self-propulsion, as well as more immersive and shaped options to accommodate the need for additional stability, postural support and comfort.
The height-adjustable shell option incorporates inbuilt growth adjustment in the back support due to the upper sliding interface.
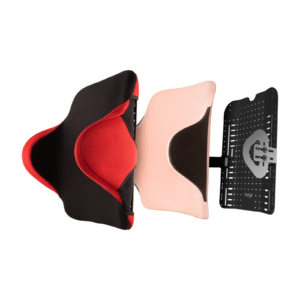
The Spex Manta is a light-weight option that provides additional lateral trunk support to users with mild trunk asymmetries or instability without compromising upper limb movement by adding additional hardware for lateral support.
The lateral ‘wings’ can be minimally adjusted. Additional shaping can be provided with positioning kits if required and if greater support is needed for the head, a head support can be fitted with ease.
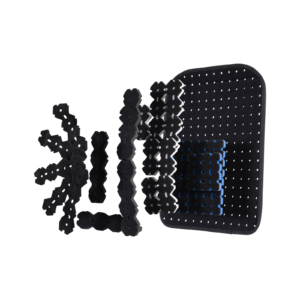
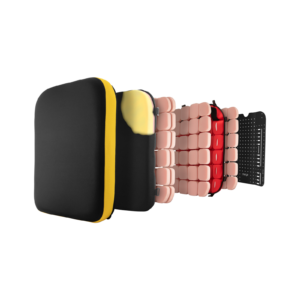
The Spex Tesselated Positioning Kit can be used with any Spex back support upholstery or under other flat foam backrest cushions to provide increased contouring for comfort and postural support.
This can be done to respond to initial assymmetry or improve comfort. This can be helpful if a user is undecided on altering an existing backrest cushion but requiring additional contouring.
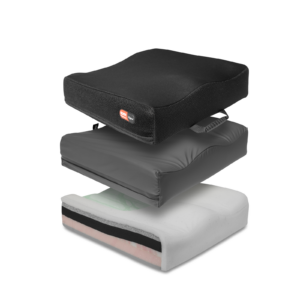
The Spex Comfi Back support is a rectangular flat cushion that can be adjusted for contouring with increased airflow for temperature control and comfort.
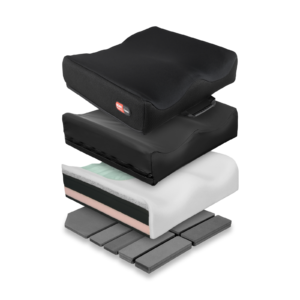
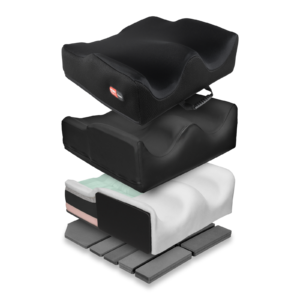
The more supportive Spex and Spex Supershape are versatile back supports that respond quickly (with easy adjustment) to more complex postural changes including posterior pelvic tilt or obliquity, spinal scoliosis
or asymmetry.
Padding components can be added from the outset or added gradually to alter the backrest cushion from a flat cushion to a contoured and shaped cushion that conforms to the user’s unique presentation.
For users who require greater immersion for comfort and postural support the Spex and Spex Supershape can provide significant support and contouring as the condition changes with easy adjustment.
All cushions include both an incontinence cover and a fabric breathable layer. All cushions have an inherent Velcro fabric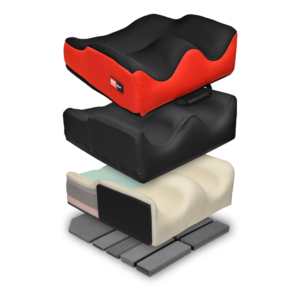 over the base to securely fix onto seat pans. Increased shaping allows for improved stability, reduced effort to sit to reduce fatigue, management of asymmetry and comfort for the user, and to support pressure management needs.
over the base to securely fix onto seat pans. Increased shaping allows for improved stability, reduced effort to sit to reduce fatigue, management of asymmetry and comfort for the user, and to support pressure management needs.
The Spex Vigour cushions provide a contoured cushion to promote comfort and posture.
The Spex contour cushions (contour, high contour and super high contour) have additional features allowing for shaping to the more complex postural presentation to promote stability at the pelvis, hips and thighs and promote comfort and pressure relief whilst influencing trunk alignment.
The Spex Flex cushion is designed to provide a stable base for those clients with a fixed hip asymmetry and obliquity. This cushion can promote a more upright posture in the trunk in sitting whilst accommodating hip flexion restrictions and can be shaped to accommodate/adjust obliquity.
The Spex lateral trunk supports, hip and medial thigh/knee supports include patented axial technology that can respond to the user’s unique postural presentation and need. There are various sizes to suit individual need. The axial technology can quickly adjust to changes in postural needs affected by tone or fatigue.
Although significant adjustment may not be required initially, these can easily be adapted to changing need. Multiple options are available for consideration and facilitate easy response to the users preferences and need.
There is a range of pelvic support belts and thoracic support harnesses to optimise stability, posture and position within the seating system.
The Spex head support range provides support in several different positions to provide optimal head alignment to encourage interaction, manage fatigue and pain and promote continued engagement in activities.
encourage interaction, manage fatigue and pain and promote continued engagement in activities.
The range includes the basic compact head support for users with good head control, the square head support, the contoured and the adjustable lateral head support for the more dependent user.
Contact us to:
- Arrange clinical education on our products in your venue of choice, or
- Obtain information about your local dealer for sales enquiries if outside of New Zealand & Australia.
Arbesman, M., & Sheard, K. (2014). Systematic Review of the Effectiveness of Occupational Therapy-Related Interventions for People With Amyotrophic Lateral Sclerosis. American Journal of Occupational Therapy, 68(1), 20–26. https://doi.org/10.5014/ajot.2014.008649
Foley, G., Timonen, V., & Hardiman, O. (2014). Understanding psycho-social processes underpinning engagement with services in motor neurone disease: A qualitative study. Palliative Medicine, 28(4), 318–325. https://doi.org/10.1177/0269216313512013
Harris, D. A. (2015). Lived-through past, experienced present, anticipated future: Understanding “existential loss” in the context of life-limiting illness. Palliative and Supportive Care, 13(06), 1579–1594. https://doi.org/10.1017/S1478951515000620
Harris, D. A. (2017). Supporting a loved one living with motor neurone disease. Palliative and Supportive Care, 15(01), 141–142. https://doi.org/10.1017/S1478951516000134
Kent, A. (2012). Motor Neurone Disease: An overview. Nursing Standard (through 2013), 26(46), 48–57.
Lau, F. S., Brennan, F. P., & Gardiner, M. D. (2018). Multidisciplinary management of motor neurone disease, 6.
Lemoignan, J., & Ells, C. (2010). Amyotrophic lateral sclerosis and assisted ventilation: How patients decide. Palliative and Supportive Care, 8(02), 207–213. https://doi.org/10.1017/S1478951510000027
MND Association. (2018). About MND. Retrieved 17 January 2019, from https://www.mndassociation.org/about-mnd/